The focus of civilized discussion of the abortion issue
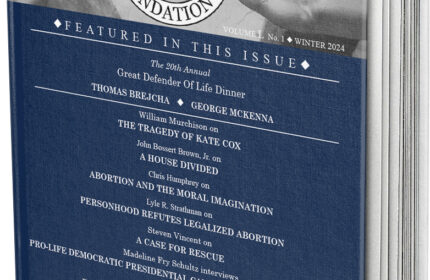
Our mission is to give the readers the tools to have a "civilized discussion" about many issues related to the life issues, most notably Abortion. Further the continuation of our cause by donating to a highly reputable life-affirming organization